Designers: Erin Graham, Michael Sakano, James Evan Smith, Brett Somocurcio
Client Coordinators: Catherine “Beth” Bale, OT, UNC Jaycee Burn Center
INTRODUCTION
At the North Carolina Jaycee Burn Center, surgeons partner with occupational and physical therapists to address the life-threatening conditions affecting their patients in tandem with therapy to improve quality of life. For patients with head and/or neck burns, lung capacity and infection may be the initial focus, but at specialty clinics like Jaycee, patients are treated to relieve the negative effects of scar formation: contracture limits joint range of motion nearby an affected area. Scar band formation distorts the typical flexibility of skin by increasing the rate of collagen deposition, causing a characteristic shortening of tissue [1, 2]. In the case of neck burns, this contracture gradually restricts the head’s natural motion, leading to loss of balance, difficulty swallowing and breathing, in addition to other factors that may reduce quality of life.
Occupational Therapists at the Jaycee Burn Center currently employ a cervical collar that mitigates scar band contracture by extending and compressing the affected area. Only two members of the occupational therapy team are able to fabricate this collar due to its complicated and specific manufacturing procedure. Thermoplastic sheets are cut roughly to size based on the judgment of the clinician and heated up for molding on the patient’s neck. Layers of padding are added for comfort and shape, then a strap is sewn to a sanitary cover and the collar is adjusted to size. This procedure takes roughly 30 minutes and many trips back and forth across the clinic. At present, fabrication is neither accessible nor efficient; improvement in either area is desired.
Additionally, the independent and qualitative determination of patient treatment status is inherently inconsistent. When assessing a patient, clinicians can only report qualitative observations and estimates of treatment status. There is no standard of measurement tracked during the patient’s treatment course [3]. As a result, the efficacy of a therapeutic approach may go unnoticed or become exaggerated. Jaycee clinicians require a tool for the objective quantification of a patient’s condition in order to determine the validity of a spectrum of treatments.
Our goal is to furnish these clinicians with tools to reduce the time spent on fabrication of collars. The less time clinicians spend making collars and in meetings, the more time they are able to spend in therapy with patients. We have developed a systematic approach to the efficient, low-cost production of a device for neck contracture rehabilitation. Additionally, we have created a tool for the objective quantification of a patient’s status over their treatment, particularly as it relates to joint range of motion and neck curvature.
SUMMARY OF IMPACT
The Occupational Therapist team at the North Carolina Jaycee Burn Center have qualitatively stated the collar provides improved benefits over the older model. As per one of the head OT members, Catherine “Beth” Bale, “most of the patients that have put this collar on have said that they liked it… and they said it feels softer… and it’s a little more form fitting or smaller for them.” From this quote, the few patients who have had access to our new product liked the feel over the original hard thermoplastic. Even if the OTs have access to only the medium sized mold, the fact that this polyurethane is flexible allows for a better fit to the contours of the neck. In addition, our application is the only one of its kind on the market. To the extent of our knowledge, this product provides state of the art, insofar as neck burn rehabilitation is concerned.
TECHNICAL DESCRIPTION
This project helps the clinicians at the Jaycee Burn Center in their efforts to provide rehabilitation to patients in two different ways. First, a collar was designed to provide compression and extension of the burned area. What makes this approach valuable is its short work time and simplicity. Any clinician will be able to quickly produce collars for their patients. Second, a tablet application was developed to allow the clinicians to capture key metrics of patient status easily and without physically touching the patient.
The first objective was to develop a systematic approach to the production of a device that mitigates neck burn scar contracture via compression and extension of the neck. The protocol for fabrication must be simple, accommodate various sizes, and the resulting collar must maintain an adequate pressure over time.
- Collar Design
The collar achieves its desired function by constituting a wedge that exerts a blanket of uniform, radial pressure on the patient’s neck. This solution is functionally consistent with pressure garment therapy, the current clinical practice for non-invasive management of hypertrophic scar bands [3,4].
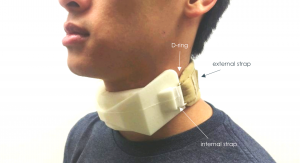
The aesthetic and comfort components of the design were conscious efforts to improve patient compliance. The flexible polyurethane foam used in this device acts as a cushion that distributes the radial pressure resulting from a strap integrated within the foam. Flex Foam-It 14 is a 2A:1B ratio liquid mix, with a working time long enough to allow thorough mixing and pouring into the custom mold [Site Flex Foam It]. The integrated strap terminates in a closed-loop fashion around D-rings that allow the attachment of a disposable external strap. Extrusions on both lateral aspects of the collar guide the internal strap placement, reduce the appearance of thin features that might compromise shear strength, and eliminate contact between the patient and D-ring that might result in pressure sores.
Additionally, cost is a key marker of this design’s success, and the selected material will run a cost of less than $10 per collar. This design can be made ahead of time, which reduces the other source of cost in the current approach – clinical billed hours.
- Fabrication Protocol
The protocol for production centers on a two-part injection mold system. Each mold consists of two halves that are secured together during casting and then separated to allow the collar to be removed in one piece. The mold halves were constructed using a fusion deposition modeling (FDM) machine to generate the negative space required to cast the collar and guidance slits for strap positioning.
The fabrication process was designed to be simple and efficient. The user positions the strap within the mold and secures with the clamp. Then foam is mixed and poured into the mold. After 30 minutes, the collar is cured to touch and can be removed from the mold. More detailed fabrication instructions can be referenced in the User Guide.
This protocol has proven to be relatively simple, efficient, and inexpensive. Standardizing this procedure has eliminated the need for excessive training and thus has made fabrication accessible to any clinician.
- Measurement Application
To provide the clinical team with a standardized method to collect patient data over the course of rehabilitation, a tablet application was developed to track neck curvature and joint range of motion (JROM). This is particularly useful for tracking neck burn rehabilitation as the patient regains the typical contour and flexibility of the neck.
The user may select to measure range of motion or cervical curvature in the sagittal plane. The application uses the tablet’s camera to capture an image of the patient from a specified angle, and this image is temporarily loaded to the application. The clinician then inputs points on the screen to mark key points and the application calculates a result. This information can be transferred to the patient’s medical record with each measurement and used to observe trends over time.
The first of the two measurements developed for this project is specifically related to neck burn rehabilitation. Curvature allows the clinician to take a picture of the patient with the camera oriented parallel to the sagittal plane and then drop multiple points along patient’s neck (Figure 6). The application then calculates a dimensionless curvature constant number based on those inputs. Tracking the contour of the patient’s neck over time is valuable in assessing the compression treatment of the collar. Theoretically over time the scar bands will reduce and the curvature constant will increase as the curve becomes more pronounced.
The second measurement developed can be applied to any joint, but is particularly relevant to neck burn rehabilitation. Joint Range of Motion (JROM) uses a similar input strategy to Neck Curvature but captures angle data from three dropped points (Figure 7). This measurement requires the image captured from a 90-degree angle to the joint and its applicable degree of freedom. For neck burn patients in particular, JROM assesses neck flexibility and head range of motion in multiple axes, two key markers of treatment progress.
In the context of burn care, patient contact is limited to prevent infection, so contact-free measurement is desirable. To the best of our knowledge, there are no existing contact-free solutions for capturing these key metrics, suggesting that our design is novel in nature. This tool has the potential to not only validate a spectrum of treatments, but also set a precedent for burn centers nationwide.




University Operator: (919) 962-2211 | © 2024 The University of North Carolina at Chapel Hill |